National Hemophilia Foundation (NHF) - Posters
A Novel Approach for Rare Bleeding Disorders: Shielded Living Therapeutics |
|
|
|
|
Objective:
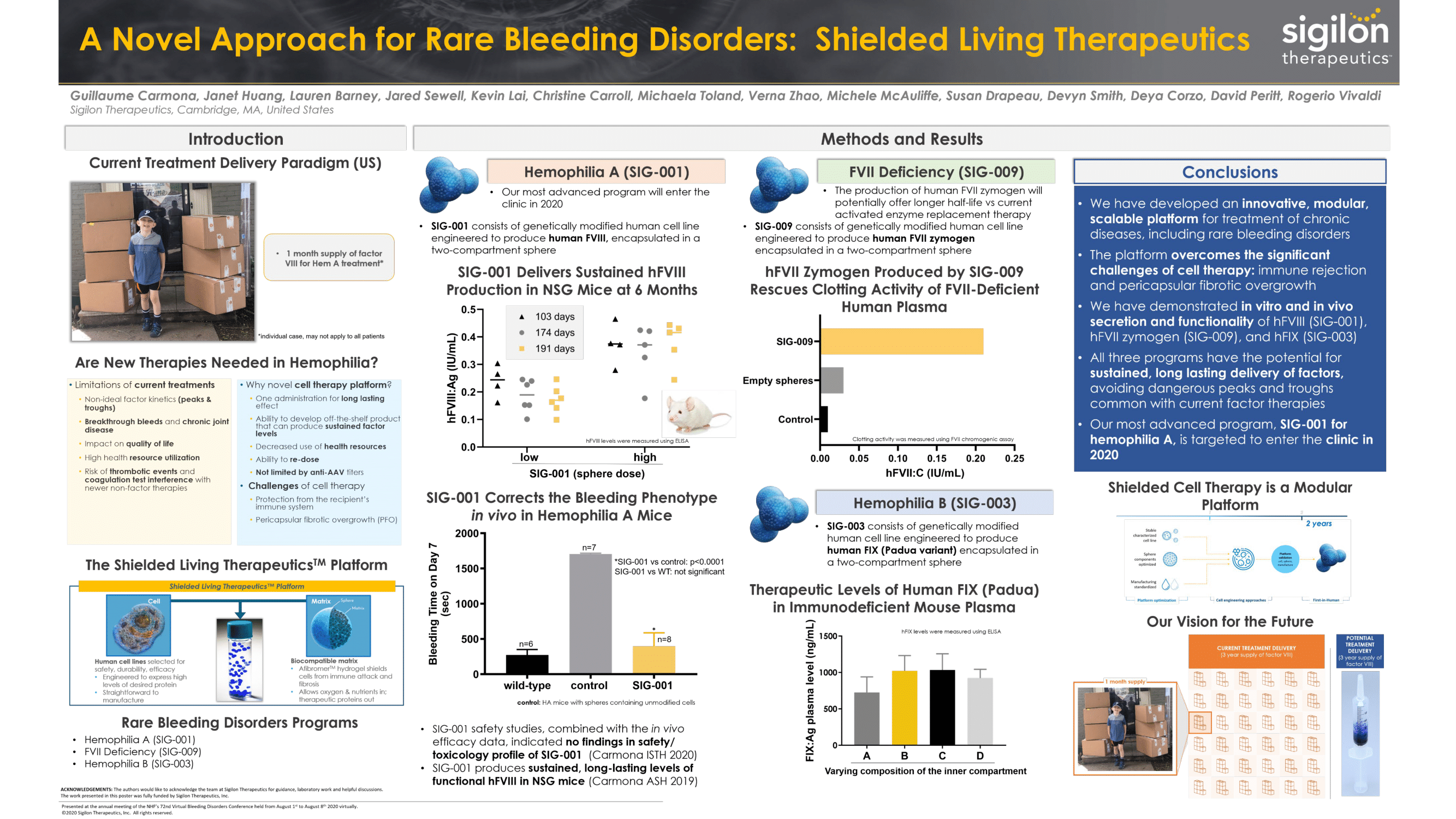
Rare bleeding disorders are currently treated with factor, and in some cases, novel non-factor therapies. While these treatments have certainly improved patient outcomes over the past few decades, there is still a need for better management of these diseases. Cell therapy is an attractive option due to the potential for continuous production of the missing protein at therapeutic levels, thus avoiding the peaks and troughs common with the factor therapies. A major challenge with such cell therapy is rejection of the allogeneic cells by the recipients immune system. We are presenting an innovative approach using cell therapy with shielded, genetically modified human allogeneic cells that candeliver long-term, sustained human factor production in vivo.
Methods:
First, we selected a non-transformed human epithelial cell line with optimal properties for encapsulation; we genetically modified this cell line ex-vivo using a non-viral vector with an optimized promoter and coding sequence for high levels of the desired factor. Next, we encapsulated the factor-expressing cells in two-compartment 1.5 mm alginate spheres. The inner compartment of the sphere contains a matrix optimized to maximize protein production by the cells when placed in vivo. The acellular outer layer contains a proprietary mixture of a novel small-molecule-modified and unmodified alginates, which minimizes the foreign body response and protects cells from contact with the hosts tissues including immune cells. The spheres in the resulting novel product are sufficiently porous to allow gasses, nutrients, and secreted proteins to freely diffuse.
Summary of Results:
Our currently disclosed rare bleeding disorder programs are: SIG-001 for hemophilia A, SIG-009 for FVII deficiency, and SIG-003 for hemophilia B. In vitro studies of non-encapsulated engineered cells demonstrated secretion and functionality of hFVIII, hFVII zymogen, and hFIX proteins, respectively. Varying doses of each final product were administered intraperitoneally (IP) to mice and showed dose-dependent circulating levels of the protein in the plasma. Long-term studies are presently being conducted to test the sustained expression of FVII and FIX in vivo. For our most advanced program, SIG-001 (hemophilia A), we conducted formal safety and toxicology studies in mice and non-human primates. These safety studies, combined with the in vivo efficacy data reported previously, indicated that no safety/toxicology signals have been identified and that SIG-001 administration resulted in sustained, long-lasting hFVIII levels in the preclinical setting. SIG-001 has been granted an orphan designation by the US FDA, and the first-in-human trial is planned to open in 2020.
Conclusions:
We aim to use this approach to develop a new category of medicines for severe chronic diseases such as hemophilia A, hemophilia B and FVII deficiency that may provide significant benefits to patients. We are working to advance the development of these programs as quickly as feasible toward clinical trials.



