National Hemophilia Foundation (NHF) - Posters
Summary of thrombotic or thrombotic microangiopathy events in persons with hemophilia A taking emicizumab |
|
|
|
|
Objective:
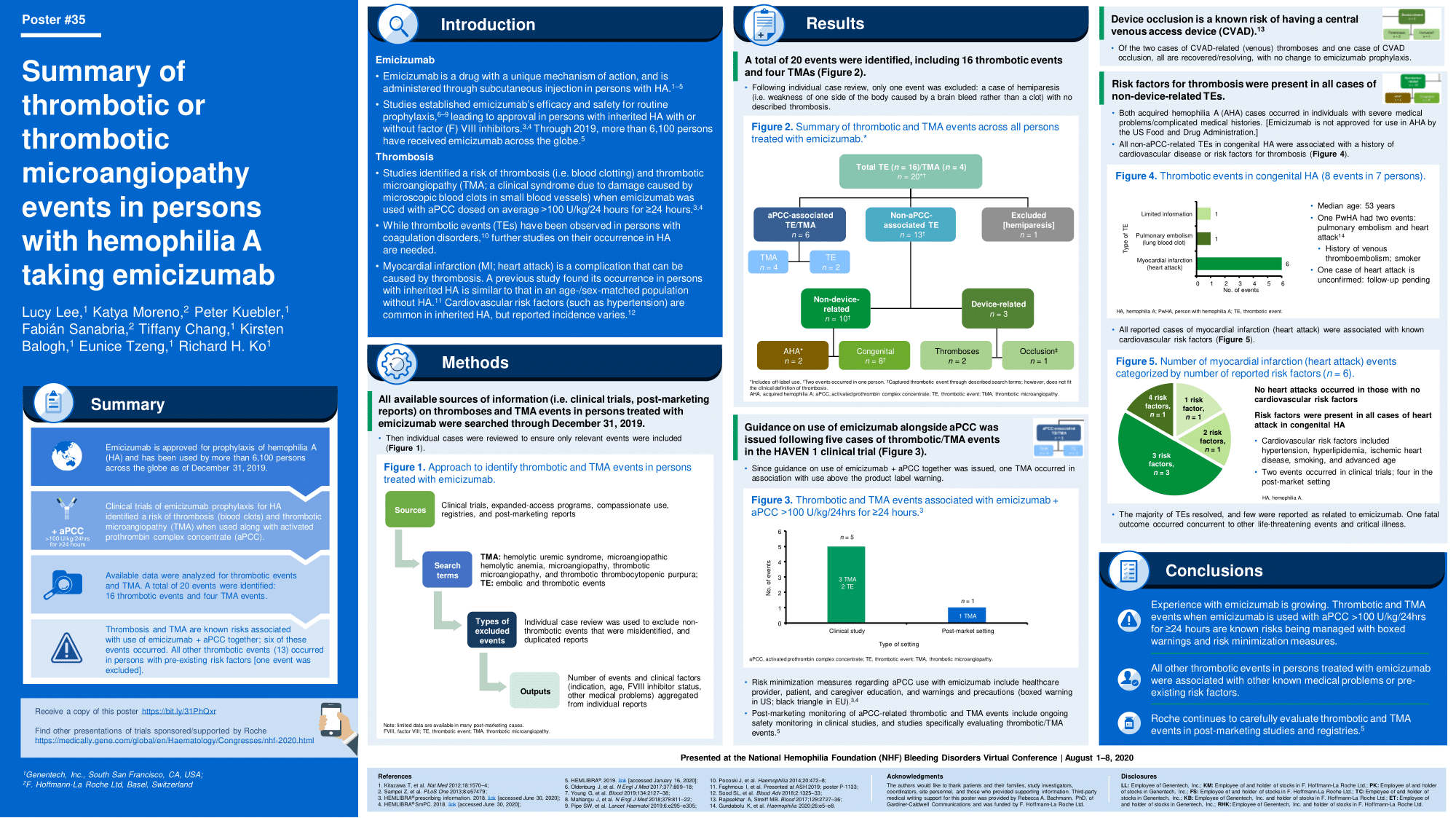
Long-term data from the HAVEN 14 clinical trials reaffirmed the safety and efficacy of emicizumab prophylaxis for persons with congenital hemophilia A. The clinical trials identified a risk for thrombotic microangiopathy (TMA; which causes damage to the lining of, and blood clots in, small blood vessels) or thrombotic (blood clotting) events when emicizumab was used alongside activated prothrombin complex concentrate (aPCC; dosed on average >100 U/kg/24 hours for ?24 hours). Emicizumab is currently approved for routine prophylaxis in persons with congenital hemophilia A with or without FVIII inhibitors, although use in persons with acquired hemophilia A (AHA), which is not an FDA-approved use, has been reported. From November 2017 through September 2019, more than 5,200 persons have received emicizumab. This analysis provides a safety evaluation of emicizumab based on available data focusing on reports of TMA and thrombotic events in persons with congenital hemophilia A or AHA.
Methods:
This summary describes data through September 30, 2019 from post-market reports, expanded access programs, compassionate use, and clinical trials. Clinical factors (indication, age, FVIII inhibitor status, comorbidities) and drug factors (co-exposure to medications that affect coagulation) were extracted from individual safety reports and aggregated. Device occlusions or non-thrombotic events misidentified with the search criteria were not included
Summary:
Among those with congenital hemophilia A who received emicizumab, there were eight thrombotic events in seven people and four TMA events in four people. All but one thrombotic event occurred in people with FVIII inhibitors. Overall, 2/8 thrombotic events were reported in persons who received aPCC alongside emicizumab; of the remaining six thrombotic events, four were clots in the arteries in persons with heart-related risk factors and two were clots in the veins in persons with blood-clotting risk factors. All TMA events occurred in patients receiving aPCC (on average >100 U/kg/24 hours for ?24 hours) alongside emicizumab. Among those with AHA, two thrombotic events occurred; one in a person with a heart-related risk factor and one in a person with a blood-clotting risk factor. Among all events, all thrombotic events and TMAs were reported as resolved or resolving. No thrombotic events or TMAs were existing in the same period as a fatality, beyond the one due to rectal hemorrhage reported previously in the HAVEN 1 clinical trial.
Conclusions:
The safety profile of emicizumab remains unchanged in congenital hemophilia A and undetermined in AHA. TMA/thrombotic events associated with emicizumab when used in combination with high-dose aPCC is an important risk and treatment consideration that warrants continued vigilance. To ensure that safety data are gathered accurately, it is important that patients/caregivers, and healthcare professionals report any event details. We continue to report TMA and thrombotic events to local regulatory authorities according to local regulations.



