National Hemophilia Foundation (NHF) - Posters
Real-world treatment patterns, health outcomes, and healthcare resource use among persons with hemophilia A |
|
|
|
|
Objective:
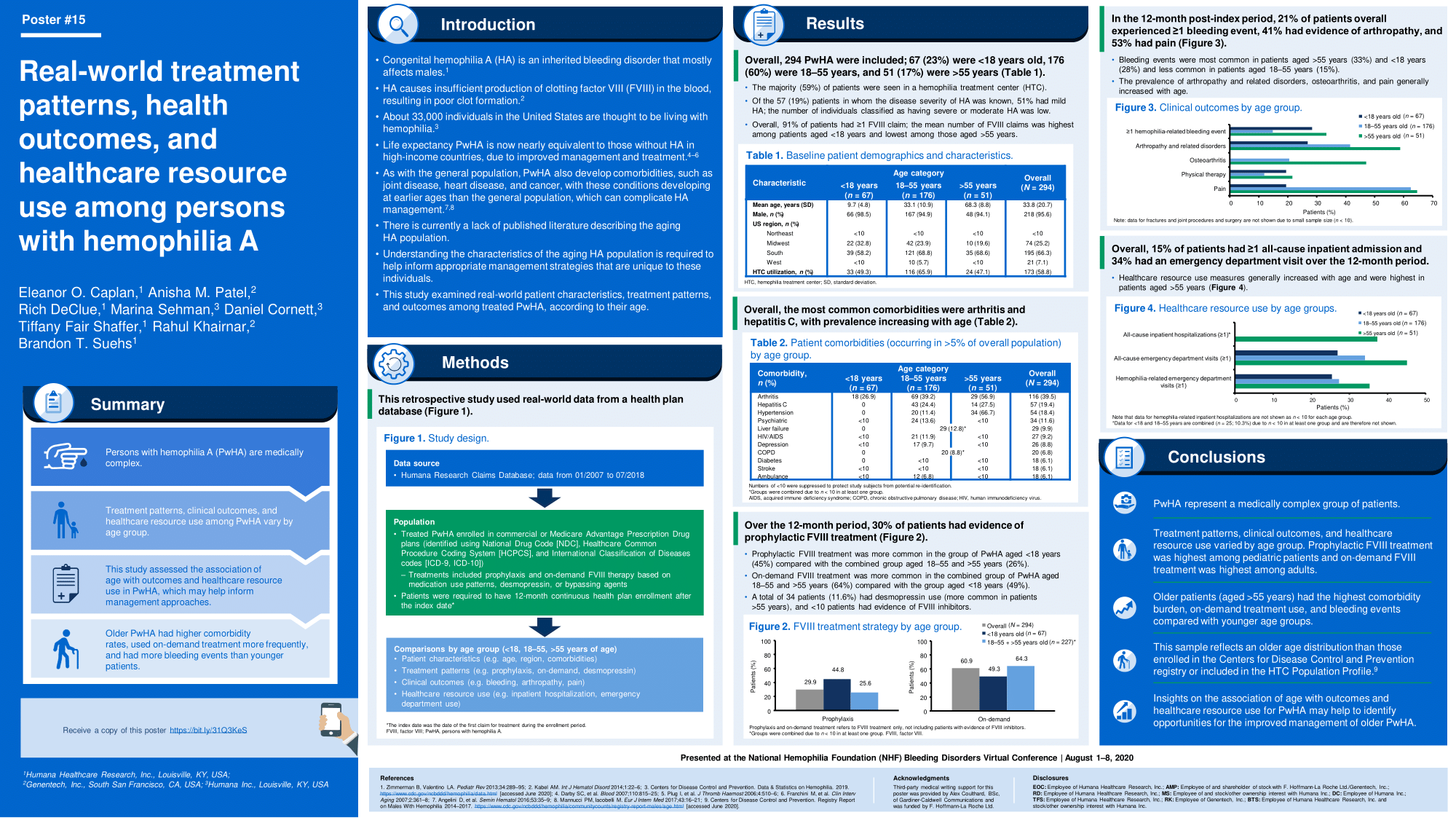
Understanding characteristics of the aging hemophilia A (HA) population is critical to informing appropriate management strategies. There is paucity of published literature describing the aging HA population. This study aims to examine real-world demographic and clinicalcharacteristics, treatment patterns, and outcomes among treated persons with hemophilia A (PwHA), stratified by age.
Methods:
This retrospective study used data from the Humana Research Database from 01/200707/2018. PwHA enrolled in commercial or Medicare Advantage Prescription Drug plans were identified based on diagnosis codes and treatments for congenital HA. Index was the first evidence for treatment during the identification period. Persons included were required to be enrolled for 12 months after inclusion in the study. Unadjusted comparisons on characteristics, clinical outcomes, and healthcare resource utilization (HCRU) were conducted across age groups (<18, 1855, >55 years).
Summary:
A total of 294 PwHA were identified; the majority were adults (1855 years=60%, >55 years=17%), males (96%), 59% were seen in a hemophilia treatment center, and 91% had ?1 FVIII claim. Overall, 30% of patients had evidence of prophylactic treatment. The most common comorbidities were arthritis (40%) and hepatitis C (19%). Severity could be identified in 19%; the majority of which were mild (50.9%). Prophylactic treatment was higher among PwHA aged <18 years (45%) compared with those aged 1855 years (31%) and >55 years (<20%), while on demand use was more common among those aged 1855 years (63%) and >55 years (69%) compared with those aged <18 years (49%). Overall, a total of 21% of patients experienced ?1 bleeding event in the 12-month post-index period, and 41% and 53% had evidence of arthropathy or related disorders, and pain, respectively; all were highest among PwHA aged >55 years. Generally, HCRU increased with age and was highest in PwHA aged >55 years.
Conclusions:
PwHA represent a medically complex group and incur substantial HCRU. Insights on differences in treatment, outcomes, and HCRU as PwHA age may identify opportunities for enhanced disease management particularly for older patients.



